Physician Compensation and the Gender Pay Gap…Yes, It Still Exists, But Not Everywhere!
Despite increased awareness and advocacy for gender equality, female physicians continue to face disparities in compensation compared to their male counterparts. According to the latest findings from Doximity’s 2025 Physician Compensation Report, the gender pay gap among physicians has not only persisted but has slightly widened over the past year. So then why is there still not only a gap, but a pretty significant one – a whopping 26% difference?
According to Doximity’s recent report and corroborated by other sources such as the American Medical Association, female physicians earn, on average, 25-30% less than male physicians. This gap persists across various specialties even when adjusting for factors such as experience, hours worked, and type of practice, discrepancies remain. However, one area in which there is NOT a gender pay gap is Locum Tenens, which is discussed later in this article.
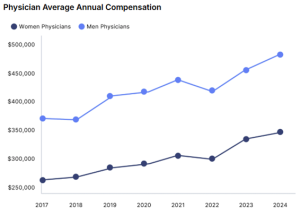
Figure 1 Source: Doximity 2025 Physician Compensation Report
Key Findings from the Report
- Overall Compensation Growth: Physician compensation in the U.S. saw a modest increase of 3.7% from 2023 to 2024. This is a decrease from the previous year’s 5.9% rise amid ongoing concerns about reimbursement cuts affecting care for Medicare and Medicaid patients.
- Gender Pay Gap Widening: The gender pay gap has returned to 26% in 2024, up from 23% in 2023, while aligning with 2022 levels. Notably, men’s pay rose by 5.7% while women’s income increased by only 1.7%. On average, women physicians earned $120,917 less than their male counterparts, even after adjusting for specialty, location, and experience.
- Annual Compensation Growth: A significant factor contributing to the widening gap is the difference in annual compensation growth between genders. Men’s substantial pay increases contribute to a growing disparity.
- Specialty Pay Gaps: Consistently, women have earned less than men across all specialties. Pediatric nephrology, for instance, has the largest gender pay gap as a percentage of pay, despite seeing substantial annual growth. Meanwhile, oncology maintains one of the smallest gaps.
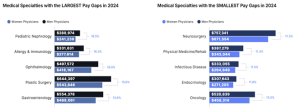
Figure 2 Source: Doximity 2025 Physician Compensation Report
- Long-term Impact: Over a 40-year career, men can make over $2 million more than women, highlighting the long-term financial implications of these disparities.
Potential Reasons for Gender Pay Gaps
- Specialty Choices: Women in medicine are often overrepresented in lower-paying specialties such as pediatrics, family medicine, and obstetrics and gynecology, while men are more prevalent in higher-paying specialties like orthopedics, cardiology, and surgery. This trend contributes significantly to the overall pay gap.
- Work-Life Balance Preferences: Studies suggest that female physicians might prioritize work-life balance more than male physicians, possibly opting for part-time positions or taking career breaks for family reasons. These choices, while valid and important, can impact overall earnings and career advancement.
- Negotiation Disparities: Research indicates that women are less likely to negotiate their salaries compared to men. This could be due to social conditioning, a lack of negotiation training, or the fear of potential backlash. Consequently, initial salary offers may set a lower baseline for women, affecting their long-term earnings trajectory.
- Discrimination and Bias: Implicit bias and discrimination, whether conscious or unconscious, still play a role in the workplace. Women might be less likely to be considered for promotions, leadership roles, or lucrative positions, which impacts their income potential.
- Organizational Policies: Some healthcare organizations lack transparent salary structures, making it difficult to identify and correct pay disparities. Without clear guidelines and accountability, gender-based pay gaps can persist unchecked.
Steps Toward Closing the Gap
Addressing the gender pay gap in medicine requires a multi-faceted approach:
- Encouraging Specialty Diversity: Promoting female representation in higher-paying specialties can help balance income disparities. This requires mentorship programs, exposure to diverse fields during medical training, and addressing any systemic barriers that deter women from pursuing certain specialties.
- Fostering Negotiation Skills: Training and workshops on negotiation can empower female physicians to advocate for themselves effectively. Organizations can play a role by offering resources and creating an environment where salary discussions are normalized and encouraged.
- Implementing Transparent Pay Structures: Healthcare organizations should adopt transparent salary frameworks and conduct regular pay audits to identify and rectify disparities. This transparency can help ensure fair compensation for all physicians, regardless of gender.
- Supporting Work-Life Integration: Healthcare organizations can offer flexible working arrangements, parental leave policies, and childcare support to accommodate physicians seeking better work-life integration without penalizing them financially.
- Consider Locum Tenens: Locum tenens agencies offer positions with standardized pay rates that are based on the role, specialty, and location, rather than the gender of the physician. This helps mitigate pay disparities that might exist in traditional permanent roles where salary negotiations can be more subjective. For example, an ER position in Massachusetts may pay a physician $330 an hour regardless of gender, thereby eliminating any pay disparity.
The gender pay gap in healthcare is a complex issue with deep-rooted causes, but it is not insurmountable. By addressing the factors contributing to these disparities and implementing needed changes, a more equitable healthcare environment can be achieved. Pay equity is not just a matter of fairness – it also reflects the values of the medical profession and enhances the quality of care for all patients. As physicians strive to heal others, let us also commit to healing the inequities within our own ranks.